Topics
10/14/2024
The Increasingly Important "Set-Point" Theory of Body Weight: What are the Environmental and Behavioral Factors?
Summary
■In 1953, Kennedy proposed that body fat storage is regulated. In 1982, nutritionists William Bennett and Joel Gurin expanded on Kennedy’s idea and developed the set-point theory. This may help explain the recurring failure of long-term dieting.
■When an individual loses weight, the body significantly reduces energy expenditure beyond what would be expected based on changes in body composition and the thermic effect of food. It also increases appetite through hormonal regulation, and alters food preferences to drive the body weight back toward a predetermined set-point range.
■Since obese individuals also exhibit these compensatory metabolic adjustments in response to dietary restriction, obesity may be considered a natural physiological state for some people.
■This body’s set-point is thought to be established early in life and remains relatively stable unless altered by specific life changes, such as marriage, childbirth, menopause, aging, or illness.
■As demonstrated in overfeeding experiments conducted in Vermont in the 1960’s, even weight gain from temporary overeating can trigger compensatory mechanisms that bring body weight back toward its set-point range.
■However, this set-point model of body weight does not explain the global rise in obesity since around 1970. Some researchers point out that while metabolic resistance to sustaining a reduced body weight is strong, its resistance to sustained fat gain may weaken over time with prolonged consumption of high-calorie foods.
< My thoughts >
■As some researchers have suggested, whether obesity as a chronic disease can be cured is depend on understanding how genetic and environmental factors interact to adjust the body's set-point weight.
■Since it is generally believed that a positive energy balance is necessary for weight gain, some researchers suggest that today’s environment of continuous high-calorie food intake may result in irreversible weight gain, which also suggests an increase in set-point weight, but I have a different view.
■There are two types of weight gain. Weight gain from temporary overeating is due to a positive energy balance, but this is usually short-term, and body weight is likely to return to its set-point.
On the other hand, I believe that long-term, irreversible weight gain, which suggests an increase in set-point weight, is more likely triggered by a negative energy balance or internal signals of “food scarcity,” similar to cases where weight increases even more after periods of starvation or dieting.
■Since 1970, one notable change in our living environment is what I call “intestinal starvation.” In many parts of the world before 1970, even if people went a whole day without eating until the next meal, there were likely still fibers and other undigested substances left in the intestines.
However, in today’s society, where easily digestible foods—such as refined carbohydrates, certain kinds of protein, and [ultra-]processed foods—are widely consumed, intestinal starvation can be induced in as little as 8 to 10 hours depending on how one eats. Through the gut-brain axis, this may send a signal to the brain indicating "there is no food."
※For an explanation of why intestinal starvation may lead to irreversible weight gain—suggesting an increase in body's set-point weight—please see Section 4.
【 Full text 】
-
Contents
-
- Advances in understanding “set-point” theory
- Problems with the set-point model
- Environmental and behavioral factors influencing weight set-point
- Why intestinal starvation increases one’s set-point weight
<How to prove my theory>
- Advances in understanding “set-point” theory
As I've explained in previous blog posts, I believe that each person has an individual “set-point” for their weight, and that understanding how this set-point increases is the key to addressing the issue of obesity.
This time, I would like to share my thoughts on recent advances in research regarding the set-point theory of body weight, as well as the environmental and behavioral factors that influence it.
1. Advances in understanding “set-point” theory
<Obesity and weight loss attempts>
♦A fat person who insists that a lean friend has consistently eaten more than the fat person does, may well be telling the truth.(*snip*)
The group of obese patients who are greatly in need of our understanding are those who keep to a calorie intake of perhaps 1000 kcal per day, yet lose less than one kg per week. There is no doubt whatsoever that such people exist, and can be studied in a metabolic ward under conditions where 'cheating' is virtually impossible without being detected. Usually these are middle-aged women who have been perhaps 40 kg overweight, and who have already lost about 20 kg. They are often depressed, hypothermic, and have a low metabolic rate. The nature of this metabolic adaptation to a low calorie diet is not known (as of 1973), but it is a phenomenon which has been known since before 1920. [1](J S Garrow, 1973)
♦For obese individuals, a certain amount of weight loss is possible through a range of treatments, but long-term sustainability of lost weight is much more challenging, and in most cases, the weight is regained [2]. In a meta-analysis of 29 long-term weight loss studies, more than half of the lost weight was regained within two years, and by five years, more than 80% of lost weight was regained [3,4].
In addition, studies of those who are successful at sustained weight loss indicate that the maintenance of a reduced degree of body fatness will probably require close attention to energy intake and expenditure, perhaps for life[5].
<Metabolic values of obese individuals>
♦The hypometabolic thesis had fallen out of favor by 1930, when more accurate calculations of body-surface area indicated that the metabolic rates of obese individuals were normal[6].
♦Total energy expenditure (TEE) in a day consists of three components: diet-induced thermogenesis (DIT), physical activity energy expenditure (PAEE), and resting energy expenditure (REE). When comparing a model case of men with an average weight of 100 kg and 70 kg, the man weighing 100 kg has a higher TEE[7] .
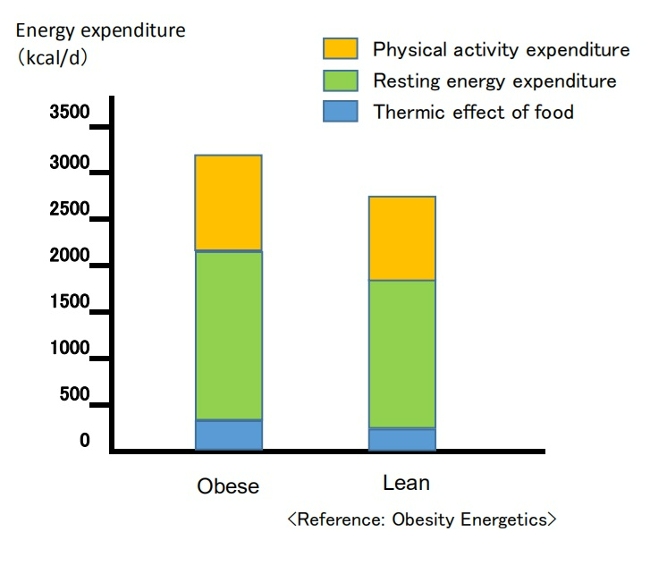
(Breakdown of energy expenditure in average 100-kg and 70-kg men)
Contrary to popular belief, people with obesity generally have a higher absolute REE compared to leaner subjects.This is because obesity increases both body fat and metabolically active fat-free mass[7,8].
PAEE can be subdivided into "voluntary exercise" and “activities of daily living.” Despite typically engaging in less physical activity, obese individuals often have a daily energy cost for physical activity similar to that of non-obese individuals since PAEE is proportional to body weight [7,9]. Additionally, due to a greater food intake, their DIT also tends to be higher [7].
<Dynamic changes in energy expenditure>
♦Obesity prevention is often erroneously described as a simple bookkeeping matter of balancing caloric intake and expenditure [10].
In this model, energy intake and expenditure are considered independent parameters determined solely by behavior. It is assumed that an obese person can steadily lose weight by eating less and/or moving more at a rate of one pound for every 3,500 kcal (or one kg for every 7,200 kcal) of accumulated dietary caloric deficit [7,11]. This view has been referred to as a “static model” of weight-loss, but it has been shown to be physiologically impossible [7,12].
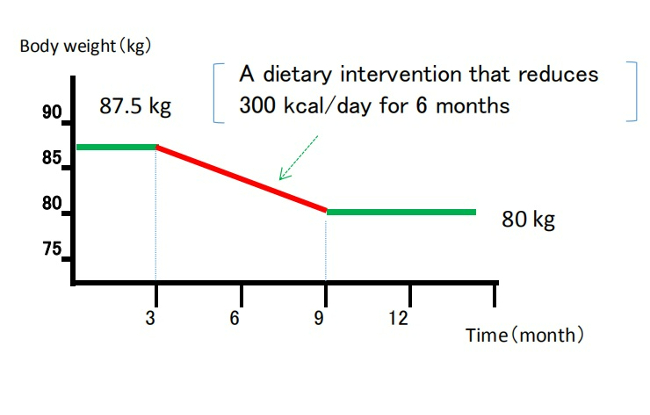
(Static model of weight loss)
(Despite being recognized as overly simplistic, the 3,500 kcal rule continues to appear in scientific literature and has been cited in over 35,000 educational weight-loss websites as of 2013.) [12,13]
♦It is now understood that energy intake and expenditure are interdependent variables, influenced by each other and by homeostatic signals triggered by changes in body weight [7,14].
Attempts to alter energy balance through diet or exercise are countered by physiological adaptations that resist weight loss [7].
<Set-point theory of body weight>
♦In recent years, the influence of homeostatic control has been recognized, and there is growing evidence that the body employs physiological mechanisms to manipulate energy balance and maintain body weight at a genetically and environmentally determined "set-point."[12]
In 1953, Kennedy proposed that body fat storage is regulated [15]. In 1982, nutritional researchers William Bennett and Joel Gurin expanded on Kennedy's concept when they developed the set-point theory [16]. The model has been widely adopted, and strengthened particularly after the discovery of leptin in the 1990’s [7,12].
When an individual loses weight, the body significantly reduces energy expenditure to a degree that is often greater than predicted based on changes in body composition and the thermic effect of food. It also causes an increase in appetite through hormonal regulation and alters food preferences through behavioral changes, to drive the body weight back toward its set-point range[7,16].
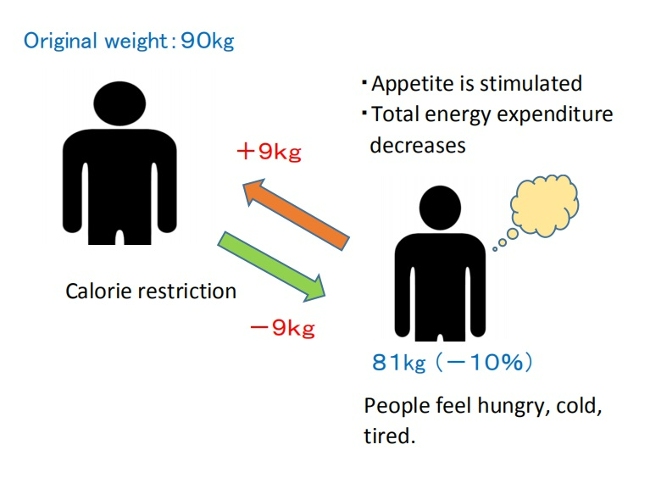
( Set-point model of weight loss)
♦Weight-loss studies have shown that the magnitude of fat stores in the body is protected by mechanisms mediated by the central nervous system, which adjust energy intake (EI) and expenditure (EE) via signals from adipose tissue, the gastrointestinal tract, and endocrine tissue to maintain homeostasis, and resist weight change (set-point model)[12,17].
♦The body's protective metabolic mechanism that attempts to preserve energy stores during an energy crisis is known as adaptive thermogenesis (AT) or metabolic adaption[7,12].
AT is defined as the underfeeding-associated fall in resting energy expenditure (REE), independent of changes in body composition[12].
♦Maintenance of a 10% or greater reduction in body weight in lean or obese individuals is accompanied by about 20 to 25% decline in 24-hour energy expenditure. This reduction in weight maintenance calories is 10 to 15% lower than what is predicted based solely on alterations (/changes) in fat and lean mass [17,18].
Since obese individuals also display these compensatory metabolic adjustments in response to dietary restriction, obesity may be considered a natural physiological state for some people. Experimental studies on obesity in animals similarly suggest a view of obesity as a condition of body energy regulation at an elevated set-point [19].
♦A meta-analysis of cross-sectional studies investigating adaptive thermogenesis (AT) by comparing formerly obese subjects who had lost weight with BMI-matched subjects who were never obese, reported a 3–5 % lower resting energy expenditure (REE) in formerly obese subjects compared to never obese controls[20].
This effect means, for example, that if an obese woman reduced her weight from 100kg to 70kg, she would have to consume fewer calories to remain at 70kg than a woman who had consistently weighed 70kg[6]. Similar results have been confirmed in animal experiments involving obese and normal-weight rats.
This suggests that the frequent claim made by obese people that they eat the same or less than their lean friends but lose no weight, must be given more credence than it is ordinarily accorded[19].
♦On the other hand, as shown in overfeeding experiments on prisoners in Vermont in the 1960’s (Doctor Ethan Sims), weight gain due to temporary overeating also triggers compensatory mechanisms that bring body weight back into a set-point range.
However, some researchers point out that these may be weaker than those protecting weight loss. This asymmetry could be due to the evolutionary advantage of storing fat to survive during periods of caloric restriction, such as prolonged starvation [16,17].

♦In addition, hyperphagia (overeating) has been demonstrated following experimental semi-starvation and short-term underfeeding, which is probably the result of homeostatic signals resulting from the loss of both body fat and lean tissue [7,21].
♦This theory also suggests that a person's set-point for body weight is established early in life and remains relatively stable unless altered by specific conditions. However, the set-point may change throughout one’s life due to factors such as marriage, childbirth, menopause, aging, and disease [16].
On the other hand, the set-point theory remains a theory because all the molecular mechanisms involved in set-point regulation have not been elucidated, and some researchers may consider this theory to be overly simplistic[16].
2. Problems with the set-point model
However, some researchers have pointed out problems with the set-point model of regulation.
If such a powerful biological feedback system regulating the state of our body fat exists, then why do many individuals in most Western countries gain weight throughout majority of their lives? In particular, they argue that this model cannot explain the increasing prevalence of obesity that has been observed in many societies worldwide since the 1970’s[22].
In response, some researchers argue that while metabolic resistance to sustaining a reduced body weight is strong, metabolic resistance to sustained increased adiposity may not be physiologically long-lasting. The steadily increasing prevalence of obesity in humans also suggests that the state of body fat is facilitated more vigorously than losing weight[17,23].
Animal studies in mice demonstrated increased energy expenditure and increased sympathetic nervous system (SNS) tone during the first 3-4 weeks of consuming a high-fat diet, while these changes were no longer evident after a few months of high-fat diet consumption[17,24].
Another animal study in mice reported that long-term consumption of palatable, high-energy diets such as potato chips, cheese crackers, cookies, etc., caused irreversible weight gain, suggesting an increase in the set-point weight[19,25]. This effect is believed to be due to the increases in the number of fat cell[19,26].

■These explanations may sound reasonable at first, but in my opinion, this is no longer a "set-point" and it fails to explain why the body stubbornly shows metabolic resistance to maintaining weight loss, even at a higher set-point weight.
When applied to humans, not everyone who frequently consumes high-calorie foods becomes obese. This brings up several contradictions, such as:
(1)Why is obesity more prevalent among the lower-income groups in Western societies[22,27] and relatively wealthier groups in developing societies?[28];
(2)The coexistence of undernutrition and obesity in poor populations, observed globally since the 1950’s[29];
(3) Why do some people gain weight after environmental changes such as entering college, getting married, having children, or moving from Asia to Western countries?[22]
As I have mentioned repeatedly in this blog, I believe that an increase in set-point for body weight is due to inducing intestinal starvation, and that I can explain all these contradictions.
In the following section, I will explain that more specifically.
3. Environmental and behavioral factors influencing weight set-point
In 2012, the American Association of Clinical Endocrinology (AACE) designated obesity as a chronic disease. One of the rationale for that designation is that, like other chronic diseases, the pathophysiology of obesity is complex, involving interactions of genetic, biological, environmental, and behavioral factors[30].
Some researchers interested in the body weight set-point theory argue that understanding how genes and the environment interact to regulate the set-point is essential to determining whether obesity, as a chronic disease, can be cured. However, they struggle to explain the many significant environmental and social influences[22].
■ I also believe that the set-point of body weight changes due to the interaction between (1) genetic and biological factors, and (2) environmental and behavioral factors, but this time, I will mainly discuss (2) in this article.
When considering changes in living environment since the 1970’s, most researchers blame the rise in obesity on the increased availability of high-calorie foods and a decrease in physical activity as society became more affluent. In other words, they believe that a positive energy balance is necessary for weight gain.
However, paradoxically, the fact that the increasing prevalence of obesity coincides with an increase in weight-loss attempts[31] suggests that our understanding of energy balance may be flawed[12].
As suggested by overfeeding experiments, “temporary weight gain from overeating” and “irreversible weight gain occurring over many years ” are different. In my view, obesity as a chronic disease arises rather from signals of negative energy balance or "food scarcity" in the body, as in the cases where people gain more weight than before after starvation or dieting.
[Related article]
The Overfeeding Study Suggests That "Overeating" Is Not the Cause of Obesity
■Despite its impact on our bodies due to changes in our living environments since the 1970’s, "intestinal starvation" remains unrecognized.
Intestinal starvation refers to a state where everything consumed is fully digested throughout the entire intestinal tract, and it can occur in today's affluent developed countries, developing countries, or even among the poor. When there is little or no fiber and everything has been digested, our bodies perceive it as having "no food."
【Related Article】
The Body Perceive That It Is More Starved than in the Past
Perhaps in many parts of the world before 1970, even if people went a whole day without eating until their next meal, there were likely still undigested substances like fiber and tough plant cell walls left in their intestines. However, in today’s society, with its abundance of easily digestible, refined carbohydrates, processed foods, and fast food, intestinal starvation can occur in as little as eight to ten hours, depending on eating habits.
Intestinal starvation is more likely to occur with frequent consumption of easily digestible refined carbohydrates (bread, noodles, rice, etc.), industrially processed meat or fish products, fast food, and snacks, etc., combined with a lack of vegetables and long periods of prolonged hunger (such as skipping breakfast, late-night meals, or irregular eating habits).
【Related Article】
■In the animal experiments on rats described in section 2 above, it was reported that consuming a "high-energy diet" for 90 days led to irreversible weight gain, suggesting an increase in the set-point. However, the "fattening” diet used in this experiment (Rolls et al., 1980) primarily consisted of highly palatable items like potato chips, cheese crackers, and cookies sold in supermarkets. Those foods contained 47.5% industrially processed refined carbohydrates (fat: 42%, protein: 10.5%) on an energy basis[25]. Moreover, rats only eat when they’re hungry, and they are capable of eating the same food repeatedly.
In contrast, the “chow” fed to the control rats may have been made from ingredients like ground wheat, ground corn, soybean meal, and fish meal, etc. In other words, just as our diets from over fifty years ago, it likely contained a high amount of indigestible components, such as fiber and tough plant cell walls.
Therefore, I question the conclusion that highly palatable "high-energy diets" alone caused the irreversible weight gain.
4. Why intestinal starvation increases one’s set-point weight
Below, I will explain the mechanism by which the set- point for body weight increases due to the induction of intestinal starvation. While some of it involves speculation, it is based on events that have happened to me several times. You may not believe it, but at least for me, it is 100% accurate.
■Let's assume there is a man who has maintained a weight of 70 kg for many years. Even though his weight may fluctuate slightly during busy periods or after overeating, his weight revolves around 70 kg, so his set-point would be considered 70 kg.
When intestinal starvation occurs, a signal that 'there is no food' is transmitted from the intestines (or small intestine) to the brain.
As a result, the body tries to absorb more nutrients, causing microscopic substances attached to the villi (or microvilli) in the small intestine to detach (Figure 1), thereby increasing the surface area for absorption and raising the absolute absorption ability.
In other words, I believe that weight gain, at least to some extent, involves not only an increase in body fat but also lean tissue such as muscle.
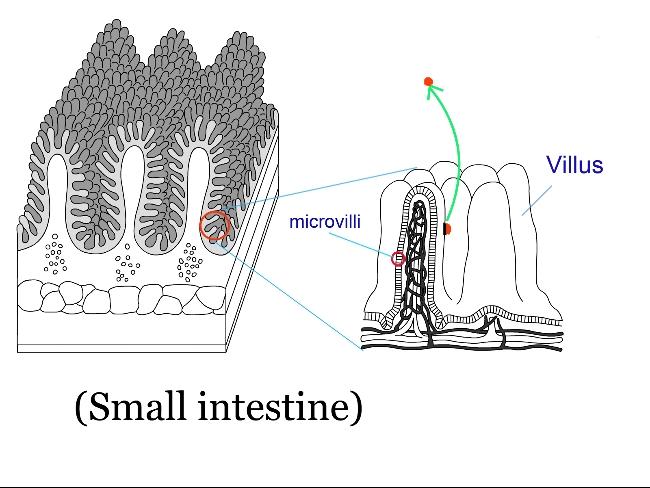
(Fig. 1 )
(Normally, a few undigested fiber or fats may remain, but when all food is perfectly digested, 5 to 10 kg of weight gain over a short period is possible.)
As a result, I believe the weight balancing point (the set-point) increases and reaches equilibrium within just a few days (Figure 2).
Weight gain does not occur from the gradual accumulation of excess calories each day, but rather in one sudden jump, possibly 0.3kg or 0.5g.
When dieting, the set-point can unknowingly rise, so you may gain a few pounds more than before once the diet ends.
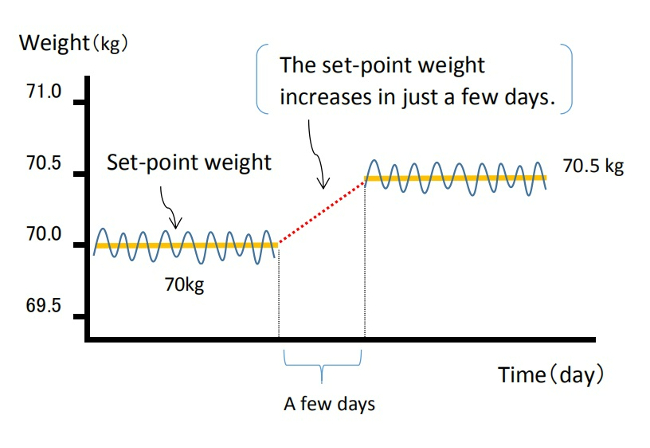
(Fig. 2 )
Once the body’s balance point rises, it becomes harder to lose weight because the overall absorption ability has increased. As mentioned in reference in section 1 , I agree with the idea that obesity is a “state of energy regulation at a higher set-point,” and is "a natural physiological condition" for obese individuals.
For more details, please refer to the article below.
【Related Article】
Gaining Weight by Intestinal Starvation; What Does It Mean?
<How to prove my theory>
It may be difficult to determine the exact cause when someone gains a few kg in a year, meaning their highest weight ever. However, I believe that, even with reduced calorie and carbohydrate intake from the meals I provide, it is possible to significantly increase a person's weight (by around 5 to 10 kg) within a few months, setting a new high set-point weight. By observing the data before and after, I think it is possible to investigate what changes have occurred inside the body.
<References>
[1]Garrow JS. Diet and obesity. Proc R Soc Med. 1973 Jul;66(7):642-4. PMID: 4741395; PMCID: PMC1645095.
[2]Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev. 2009;10(3):313–323.
[3] Hall KD, Kahan S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med Clin North Am. 2018 Jan;102(1):183-197.
[4]Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001 Nov;74(5):579-84.
[5]Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323-41.
[6]Jou C. The biology and genetics of obesity--a century of inquiries. N Engl J Med. 2014 May 15;370(20):1874-7.
[7]Hall KD, Guo J. Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition. Gastroenterology. 2017 May;152(7):1718-1727.e3.
[8]Nelson KM, Weinsier RL, Long CL, et al. Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr. 1992;56:848–856.
[9]Westerterp KR. Physical activity, food intake, and body weight regulation: insights from doubly labeled water studies. Nutr Rev. 2010;68:148–154.
[10] Levine DI. The curious history of the calorie in U.S. policy: a tradition of unfulfilled promises. Am J Prev Med. 2017;52:125–129.
[11] Hall KD, Chow CC. Why is the 3500 kcal per pound weight loss rule wrong? Int J Obes (Lond). 2013 Dec;37(12):1614.
[12] Egan AM, Collins AL. Dynamic changes in energy expenditure in response to underfeeding: a review. Proc Nutr Soc. 2022 May;81(2):199-212. doi: 10.1017/S0029665121003669. Epub 2021 Oct 4. PMID: 35103583.
[13]Thomas DM, Martin CK, Lettieri S et al. (2013) Can a weight loss of one pound a week be achieved with a 3500-kcal deficit? Commentary on a commonly accepted rule. In Int J Obes 37, 1611–1613.)
[14]Hall KD, Heymsfield SB, Kemnitz JW et al. Energy balance and its components: implications for body weight regulation. Am J Clin Nutr. 2012 Apr;95(4):989-94.
[15]KENNEDY GC. The role of depot fat in the hypothalamic control of food intake in the rat. Proc R Soc Lond B Biol Sci. 1953 Jan 15;140(901):578-96.
[16] Ganipisetti VM, Bollimunta P. Obesity and Set-Point Theory. 2023 Apr 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 37276312.
[17] Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. Int J Obes (Lond). 2010 Oct;34 Suppl 1(0 1):S47-55.
[18] Leibel R, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Eng J Med. 1995;332:621–28.
[19] Richard E. Keesey, Matt D. Hirvonen, Body Weight Set-Points: Determination and Adjustment, The Journal of Nutrition, Volume 127, Issue 9, 1997, Pages 1875S-1883S, ISSN 0022-3166.
[20]Astrup A, Gøtzsche PC, van de Werken K, et al. Meta-analysis of resting metabolic rate in formerly obese subjects. Am J Clin Nutr. 1999 Jun;69(6):1117-22.
[21] Dulloo AG, Jacquet J, Girardier L. Poststarvation hyperphagia and body fat overshooting in humans: a role for feedback signals from lean and fat tissues. Am J Clin Nutr. 1997;65:717–723.
[22]Speakman JR, Levitsky DA, Allison DB, et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech. 2011 Nov;4(6):733-45.
[23] Schwartz MW, Woods SC, Seeley RJ, et al. Is the energy homeostasis system inherently biased toward weight gain? Diabetes. 2003 Feb;52(2):232-8.
[24] Corbett SW, Stern JS, Keesey RE. Energy expenditure in rats with diet-induced obesity. Am J Clin Nutr. 1986 Aug;44(2):173-80.
[25] Rolls B.J., Rowe E.A., Turner R.C. Persistent obesity in rats following a period of consumption of a mixed high energy diet. J Physiol. 1980 Jan;298:415-27.
[26]Faust I.M., Johnson P.R., Stern J.S., Hirsch J. Diet-induced adipocyte number increase in adult rats: a new model of obesity. Am. J. Physiol., 235 (1978), pp. E279-E286
[27] Dykes J et al. Socioeconomic gradient in body size and obesity among women: the role of dietary restraint, disinhibition and hunger in the Whitehall II study. International Journal of Obesity 2004 Feb,:262-68.
[28] Poskitt EM. Countries in transition: underweight to obesity non-stop? Ann Trop Paediatr. 2009 Mar;29(1):1-11.
[29] Gary Taubes. 2011. Why we get fat. New York: Anchor Books, Pages 31-40.
[30]Garvey WT. Is Obesity or Adiposity-Based Chronic Disease Curable: The Set Point Theory, the Environment, and Second-Generation Medications. Endocr Pract. 2022 Feb;28(2):214-222.
[31]Montani JP, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk? Obes Rev. 2015 Feb;16 Suppl 1:7-18.